Let's talk about the vaginal microbiome
- cambridgefemtech
- 25 mar 2024
- Tempo di lettura: 5 min
Contributed article by Alessia Squitieri
Trillions of microorganisms are present in the human body, colonising our gut, skin, mouth, respiratory and reproductive tracts. It is estimated that microbes approximately account for about 1 to 3 percent of the human body's mass [1]. The vaginal mucosa is characterised by a stratified, squamous, non-keratinized epithelium covered by cervicovaginal secretions. Due to its limited blood supply, it receives oxygen, glucose, and other nutrients from underlying submucosal tissues via diffusion, resulting in a relatively anaerobic environment. The vagina contains a complex microbial community that subsists in a symbiotic relationship with the host. Unlike the gut microbiome, characterised by high diversity of microbial species, women's vaginal microbiome is characterised by a lower microbial diversity. This characteristic made the vaginal microbiome a sensitive and dynamic microenvironment, that responds to lifestyle and hormonal changes like pregnancy, menstrual cycle, and contraceptive use [2]. The vaginal microbiome is composed of the indigenous environment, microorganisms, and their genomes as a whole and it is dominated by bacteria from the genus Lactobacillus spp, which maintain a healthy microbiome and protect against pathogens. Additionally, Lactobacillus spp is the primary producer of L-lactic acid and D-lactic acid, which maintain the pH level in the environment below 4.5 [3]. However, this delicate microenvironment dominated by Lactobacillus spp can be easily disrupted, causing vaginal inflammation and boosting the probability of developing vaginal health problems, such as bacterial vaginosis (BV), candidiasis (thrush), and sexually transmitted infections (STIs) [2,3].
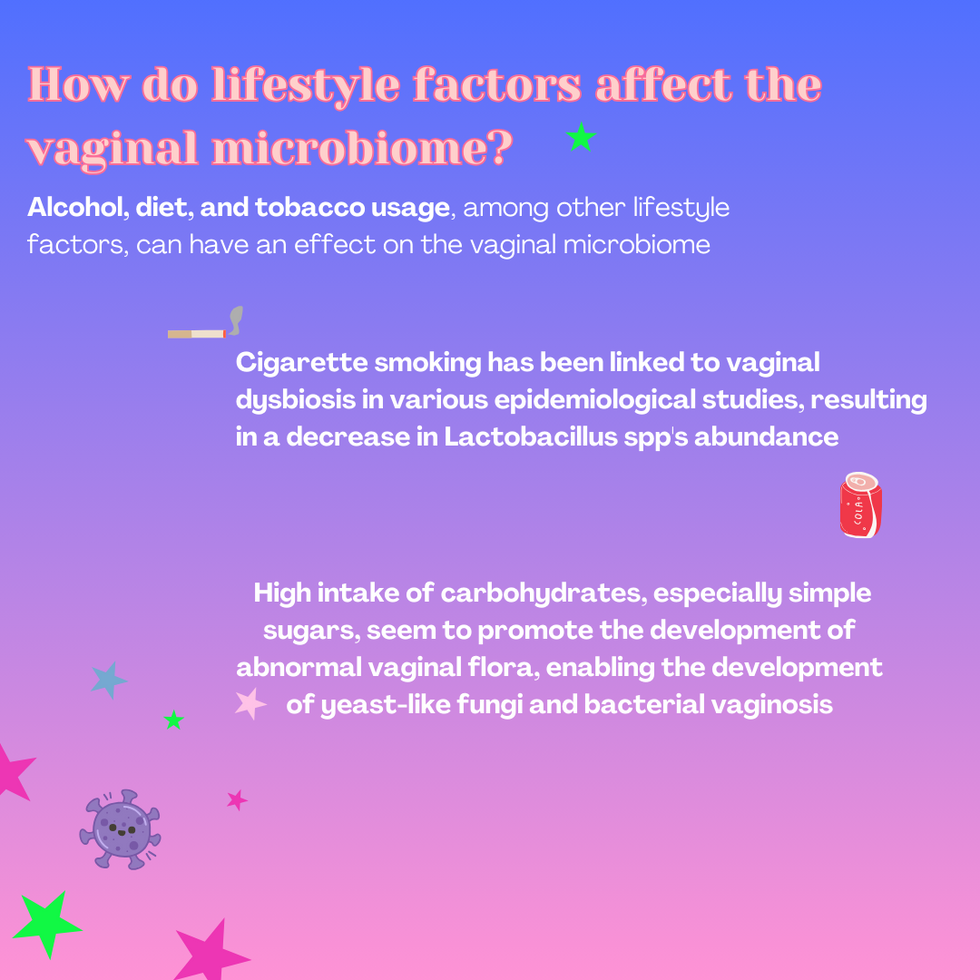
Alcohol, diet, and tobacco usage, among other lifestyle factors, can have an effect on the vaginal microbiome. Cigarette smoking, for example, has been strongly correlated with vaginal dysbiosis in different epidemiological studies. Researchers have observed that smokers' vaginal microbiota are significantly more likely to be in a low-lactobacillus state than non-smokers [4]. Diet plays a crucial role in the vaginal microbiome’s composition too. High intake of carbohydrates, especially simple sugars, seem to promote the development of abnormal vaginal flora, enabling the development of yeast-like fungi [5] and BV conditions. In both cases, a low abundance of Lactobacillus spp has been described. On the other hand, having a balanced diet and increasing the intake of micronutrients such as vitamin E, folate, and calcium have been described to reduce the risk of severe BV by 60% [2].
Surprisingly, most of the common hygiene products and practices chosen by women to remove discharge and odour from their genital area seem to be risky for the vaginal microbiome. American and African women frequently use vaginal douching to clean up, prevent or treat odour and infections, and after sexual intercourse and menstruation. However, the use of vaginal douching has been associated with BV, pelvic inflammatory disease, preterm birth and infertility [14]. Moreover, the use of products such as washes, gels and lubricants among others, appear to reduce the abundance of Lactobacillus spp, improving the odds of having vaginal dysbiosis and facilitating sexual and non - sexual infections [15]. To establish the correct vaginal hygiene practices that women should follow, additional research is needed. At present, the use of vaginal douches is well-established as having multiple negative side effects, so it is recommended to avoid or reduce its use. [2]
Hormonal fluctuations also affect the vaginal microbiome. Different studies have reported consistent findings of Lactobacillus-depletion during menses. It seems that before the start of the period, vaginal microbial diversity increases, with a concurrent decrease in Lactobacillus. On the other hand, during ovulation, when oestrogen levels are highest, a shift towards Lactobacillus-dominance has been found [2,5]. Regarding the use of hormonal contraceptives, there is not a direct correlation between their use and vaginal dysbiosis. A study conducted by Song et al., suggests that women not using hormonal contraceptives and those using combined contraceptives have similar periodic fluctuations of vaginal microbiota, corresponding to phases of the menstrual cycle. However, in the same study, women using progestin-only local release contraceptives, without a hormone-free period, have shown a disruption of the vaginal microbiota and a suppression of Lactobacillus growth [5].
Polycystic ovary syndrome (PCOS) is a complex condition that affects women worldwide. The PCOS impacts metabolic, reproductive and endocrine systems and it is esteemed to be one of the leading causes of infertility in women. Different studies [8,9] have reported a vaginal dysbiosis in PCOS patients, probably due to the hormonal imbalance that causes a reduction of oestrogen levels, reducing the abundance of Lactobacillus. Moreover, the gut microbiome also appears to be different in PCOS patients. Studies suggest that patients show an increase of Prevotella, Bacteroides, and Escherichia and a reduction of Lactobacillus and Bifidobacteria. Thanks to the existing correlation between the gut microbiome and the reproductive one, through the gut - vaginal axis, it’s also likely that PCOS-related disruptions of the gut microbiome could impact the vaginal microbiome [9]. Endometriosis is a chronic condition that affects 10% of women in reproductive age and that is still so hard to be diagnosed. Unfortunately, there are not enough studies to suggest a direct correlation between microbiome dysbiosis and endometriosis but, a recent study evidenced that Fusobacterium bacteria might be linked to endometriosis. In this study, Fusobacterium was found in over 60% of women with endometriosis and only in 7% of women without endometriosis. However, more research is needed to figure out exactly how endometriosis and dysbiosis are linked [10].
Most interestingly, the vaginal microbiome has been demonstrated to influence the outcomes of in vitro fertilisation (IVF). Specifically, it seems that the microbiome profile that supports pregnancy was dominated by Lactobacillus spp. The correlation between pregnancy outcomes and women’s vaginal microbiome is so strong that it can be used to predict the success of the treatment with an accuracy of 94% [7].
Juno Bio [11], is a start-up based in the UK that has developed an at - home test to decode the vaginal microbiome. They use innovative bioinformatics tools to predict the vaginal microbiome composition and help women to better understand their condition. Evvy [12] is a US company unlocking precision women’s healthcare through novel female biomarkers, starting with the vaginal microbiome. Freya biosciences [13] is a clinical-stage company taking an innovative approach to women’s health, with microbial immunotherapies aimed at relieving the chronic inflammation underlying a range of reproductive system diseases uniquely afflicting women.
References
NIH Human Microbiome Project defines normal bacterial makeup of the body
Holdcroft AM, Ireland DJ, Payne MS. The Vaginal Microbiome in Health and Disease—What Role Do Common Intimate Hygiene Practices Play? Microorganisms. 2023; 11(2):298. https://doi.org/10.3390/microorganisms11020298
Chen X, Lu Y, Chen T, Li R. The Female Vaginal Microbiome in Health and Bacterial Vaginosis. Front Cell Infect Microbiol. 2021;11:631972. doi: 10.3389/fcimb.2021.631972.
Lewis FMT, Bernstein KT, Aral SO. Vaginal Microbiome and Its Relationship to Behavior, Sexual Health, and Sexually Transmitted Diseases. Obstet Gynecol. 2017 Apr;129(4):643–654. doi: 10.1097/AOG.0000000000001932. PMCID: PMC6743080. NIHMSID: NIHMS1049888. PMID: 28277350.
Mizgier M, Jarzabek-Bielecka G, Mruczyk K, Kedzia W. The role of diet and probiotics in prevention and treatment of bacterial vaginosis and vulvovaginal candidiasis in adolescent girls and non-pregnant women. Ginekol Pol. 2020;91(7):412-416. doi: 10.5603/GP.2020.0070. PMID: 32779162.
Song SD, Acharya KD, Zhu JE, Deveney CM, Walther-Antonio MRS, Tetel MJ, Chia N. Daily Vaginal Microbiota Fluctuations Associated with Natural Hormonal Cycle, Contraceptives, Diet, and Exercise. mSphere. 2020 Jul 8. doi: 10.1128/msphere.00593-20
Jin C, Qin L, Liu Z, Li X, Gao X, Cao Y, Zhao S, Wang J, Han T, Yan L, Song J, Zhang F, Liu F, Zhang Y, Huang Y, Song Y, Liu Y, Yao Z, Chen H, Zhang Z, Zhao S, Feng Y, Zhang YN, Qian Y, Sun T, Feng Q, Zhao H. Comparative analysis of the vaginal microbiome of healthy and polycystic ovary syndrome women: a large cross-sectional study. Reprod Biomed Online. 2023 June 1. doi: 10.1016/j.rbmo.2023.02.002
Muraoka A, Suzuki M, Hamaguchi T, Watanabe S, Iijima K, Murofushi Y, Shinjo K, Osuka S, Hariyama Y, Ito M, Ohno K, Kiyono T, Kyo S, Iwase A, Kikkawa F, Kajiyama H, Kondo Y. Fusobacterium infection facilitates the development of endometriosis through the phenotypic transition of endometrial fibroblasts. Sci Transl Med. 2023 Jun 14;15(700):DOI: 10.1126/scitranslmed.add1531.
Baird, D. D., Weinberg, C. R., Voigt, L. F., & Daling, J. R. (1996). Vaginal douching and reduced fertility. American Journal of Public Health, 86(6), 844-850. https://doi.org/10.2105/AJPH.86.6.844
Fashemi, B., Delaney, M. L., Onderdonk, A. B., & Fichorova, R. N. (2013). Effects of feminine hygiene products on the vaginal mucosal biome. Article: 19703. Received 19 Sep 2012, Accepted 21 Jan 2013, Published online: 25 Feb 2013.





















Commenti